Tuesday Tips
2024
Did You Know?
Tuesday Tips are based on research questions from our community of LAT Compendium subscribers. You are not alone! Finding the right case doesn’t have to be a challenge. Let inHEALTH’s Live Chat experts help you find what you need.
December Tips
Calling All Motions!
Q: I am filing a motion requesting surveillance evidence to be admitted after the production deadline. Can you provide me with cases in favour of my request?
Motions before the LAT are often combined with the hearing decision. However, stand-alone motions are often not published on CanLii and are generally only provided to the parties. They are not included in the LAT Compendium unless submitted to inHEALTH by one of the parties.
Tip: Provide inHEALTH with your motion decisions received by the LAT. inHEALTH will add a case summary and organize the relevant data into our database making important issues available and searchable. Share your motion results by submitting your decision to service@inhealth.ca.
Login to inHEALTH’s LAT Compendium:
1. Go to Keyword search
2. Search: Surveillance
3. Filter by “Issues”: Evidence-Admissibility
4. Results: 57 decisions on inHEALTH’s LAT Compendium. (filtering by “Case Type: Motion” brings the results to 2. Your submitted motion decisions will allow us to increase this number.)*
*Stand-alone motions can be filtered by selecting “Case Type”: Motion.
|
19-012281 v Wawanesa: At the outset of the hearing, Adjudicator Paluch considered the Applicant’s request to exclude the Respondent’s surveillance report and social media searches as they were served two and a half months late. Finding said evidence to be relevant, the Adjudicator declined the request but allowed parties to file submissions on its weight at the conclusion of the hearing. 19-014590 v TTC: Adjudicator Lester agreed with the Applicant that the video and report give very little probative value and are not relevant to the issues in dispute. The video was not used to determine the benefits in dispute and was not given to any of the assessors for comment. The Respondent had the video and report for 3 years and it missed two ordered deadlines to produce it. The three cases relied on by the Respondent were found to be distinguishable as the video surveillance was considered relevant to the issues in dispute in those cases. In this case, the prejudice caused to the Applicant in preparing its witnesses and elongating the hearing outweighs any probative value and therefore it was excluded. 20-000829 v Aviva: The Tribunal found that the surveillance evidence obtained by the Respondent is not admissible due to late submission. The Tribunal found the Respondent did not take any steps to rectify its error and instead placed the onus on the Applicant to relieve the Respondent of its obligations to provide proper disclosure of evidence and provide her with the opportunity to deny, explain or adopt the evidence.
|
|
21-011865 v Security National: The Respondent submitted that the surveillance should not be excluded as it was served 10 days in advance of the hearing. Further, the surveillance was just obtained recently and was relevant to the Applicant’s function. Adjudicator Hines admitted the surveillance and advised that any relevance of the evidence would go to weight. 22-001330 v Co-operators: Addressing the procedural issue first, Adjudicator Adamidis accepted the Applicant’s request to exclude the surveillance report dated December 2021 because it was submitted past the deadline set by the CCRO and the Respondent provided no explanation for its non-compliance. |

Do You Know What You Missed Last Week?
Q: I don’t want to miss important new LAT and court decisions, but I just don’t have the time to read them all. How can inHEALTH help me with this?
In the ever-evolving landscape of Accident Benefit disputes, with an average of 30 decisions released weekly by the LAT and courts, staying up to date with current case law and interpretation is crucial to all practicing professionals who want to maintain a competitive edge and deliver the best results.
inHEALTH’s LAT Compendium’s comprehensive/nuanced case summaries help you stay current as fast and effectively as possible.
Here are a few reasons why staying up to date is critical:
- Changes in Legal Precedent: Each decision can either reinforce or alter established principles, which may shift how claims are handled. Keeping up with rulings ensures that you are considering the most current interpretations and precedents.
- New Ideas to Bring to Your Files and Inform Strategy: Understanding how the LAT and the courts are interpreting the SABS ensures that you can make decisions that are aligned with current case law. Keeping up with decisions gives you new ideas to apply to your own files and helps in negotiating settlements, providing advice, and preparing for hearings.
- Adapting to Evolving Standards: The legal landscape often reflects broader societal changes, such as shifts in medical practices, insurance trends, or public policy. Accident Benefit decisions can adapt to these, influencing claim assessments, benefit eligibility, and compensation calculations.
Tip: Use inHEALTH’s LAT Compendium “Recently Added” tab to view all decisions published in the last 30 days (or set a custom date range).
Talk to your personal support team on Live Chat. We provide answers
Login to inHEALTH’s LAT Compendium:
1. Go to the ‘RECENTLY ADDED’ Tab
2. Results: 100 decisions on inHEALTH’s LAT Compendium
3. Skim the “Issues” listed and decide which cases you want more details on
4. Click “Read more” to get a further layer of information and use the save/print feature for an added bonus!
23-015303 v Zenith Insurance: The Tribunal found the Applicant was involved in an accident on September 16, 2020, within the meaning of s.3(1). The Applicant’s injuries occurred when she fell while attempting to walk her dog around a parked truck that was overhanging the sidewalk. The Tribunal found that although her dog, the uneven sidewalk, or her sandal may have contributed to her subsequent injury, the use or operation of the pickup truck, parked so that its bumper was overhanging the sidewalk requiring her to attempt to navigate around it, was a direct cause of her injury. Navigating around the bumper of a parked truck is a normal incident of the risk involved in using the vehicle. The Applicant met both the purpose and causation test.
TD Insurance v 21-013393: The Applicant (the insurer) was entitled to seek repayment of medical and rehabilitation benefits paid due to the Respondent’s (the insured) material misrepresentations pursuant to s. 52 of the Schedule. The Tribunal rejected the Respondent’s argument that no repayment was owed for benefits paid directly to third-party service providers. It was persuaded by the Tribunal cases provided by the Respondent that found claimants were liable to repay medical and rehabilitation benefits, regardless of if the payments went directly to third-party service providers, because they were consistent with the intentions of s. 52. It found it would be illogical to consider that the intention of the legislature was to limit an insurer’s ability to claim repayment if the benefits were paid directly to third-party service providers.
22-004678 v Aviva: Adjudicator Levitsky applied the principles in the Divisional Court decision in Zheng, Cai v. Aviva , which found that s.38 referred to the specific Treatment Plan in question, and s.38(11) did not impose a permanent prohibition on an insurer with regard to a MIG determination. Adjudicator Levitsky found that an improper denial did not result in the Applicant being removed from the MIG entirely.

Can One Mistake Take You Out of the MIG?
Your inHEALTH team has noticed that in several recent decisions, the Applicant argued that a s.38(8) notice violation allowed them to be removed from the MIG pursuant to s.38(11)1. The section reads:
“38(11) If the insurer fails to give a notice in accordance with subsection (8) in connection with a treatment and assessment plan, the following rules apply:
1. The insurer is prohibited from taking the position that the insured person has an impairment to which the Minor Injury Guideline applies.”
While one reading of the section could suggest that a notice violation takes the Applicant out of the MIG entirely, and some early Tribunal decisions interpreted it this way, the Divisional Court in Zheng and Cai v. Aviva held that s.38(11)1 only prohibits the insurer from applying the MIG to the Treatment Plan the violation relates to because the language used in s.38 refers to a specific Treatment Plan submission.
Tip: We have several “Non-Compliance” filters that you can use, including one for s.38(11) violations. You can also use our date filter to find recent decisions that have involved this issue.
Talk to your personal support team on Live Chat. We provide answers
- Go to Advanced Search
- Select Primary Criteria “Issues/Benefit in Dispute”: Non-Compliance S.38(11)
- Select Secondary Criteria “Issues/Benefit in Dispute”: MIG
- Filter by “Release Date”: 2022-12-10 to 2024-12-10
Results: 36 decisions on inHEALTH’s LAT Compendium
21-012748 v Aviva: Adjudicator Deol applied the 2018 Divisional Court Decision of Zheng Cai v. Aviva, where the language of s.38(11) operated to bar the Respondent from taking the MIG position in respect of the particular Treatment Plan and was not an absolute bar in relation to the entire Application. Adjudicator Deol found that the Applicant was entitled to any incurred costs between the time period starting on the 11th business day after the day the Respondent received the Treatment Plan and ending on October 19, 2021.
22-007295 v Belairdirect: The Applicant was found to be in the MIG because he produced no substantive submissions or evidence but relied solely on his argument that he should be removed pursuant to s.38(11) of the Schedule due to the Respondent’s breach of the notice requirements set out in s.38(8). However, the Tribunal found that Zheng and Cai v. Aviva held that s.38(11) only applied to the specific Treatment Plan in question and did not impose a permanent prohibition on the insurer applying the MIG.
22-008578 v Allstate: Adjudicator Levitsky applied the principles in the Divisional Court decision in Zheng, Cai v. Aviva , which found that s.38 referred to the specific Treatment Plan in question, and s.38(11) did not impose a permanent prohibition on an insurer with regard to a MIG determination. Adjudicator Levitsky found that an improper denial did not result in the Applicant being removed from the MIG entirely.

S.44 Insurer Exams - How Often is Too Often?
Q: I’m looking for cases that deal with the frequency upon which an insurer can examine the insured on the same benefit.
Section 44, “Examination Required by Insurer” allows an insurer, “not more often than is reasonably necessary “ to have an insured person examined. The LAT has fleshed out a Reasonably Necessary test in two key decisions: Al-Shimasawi v. Wawanesa and 16-003144 v. CUMIS General Insurance.
Tip: Did you know that inHEALTH has developed a large list of ‘issue filters’ based on our extensive knowledge of the SABS? For this question, we were able to narrow the search by starting with the ‘Reasonably Necessary Test (S.44)’ issue. Alternatively, we could do a ‘Referenced Cases’ search for the two key cases: Al-Shimasawi v. Wawanesa and 16-003144 v. CUMIS.
Talk to your personal support team on Live Chat. We provide answers
- Go to Benefit/Issue Search
- Select Issues/Benefit in Dispute: Reasonably Necessary Test (S.44)
- Filter results by “Favour of Decision”
Results: 12 decisions on inHEALTH’s LAT Compendium
16-003144 v Cumis: In balancing these rights, a number of factors can be considered. There must be a reasonable nexus between the type of examination requested and the claimed impairments. The purpose and timing of the request should be considered. Insurer’s examinations should be for the purpose of adjusting the claim, not solely to bolster a case for litigation. Some other factors to consider include the number and nature of previous and requested examinations, whether there are new conditions that need to be evaluated, and whether either side will be prejudiced by the examination or non-compliance with a request for an examination. If there are numerous examinations, the insurer should proceed cautiously, as all of the assessments may not be necessary. There must also be an acceptable reason for non-compliance with requests for insurer’s examination requests, such as a medical reason for non-attendance.
21-005342 v Intact: The Tribunal found it would be prejudicial to the Applicant to undergo another psychological IE following the death of the initial assessor Dr. Kiss, and that the complete file and raw psychological test data had been provided to Psychologist Dr. L. Davidson. In Dr. Davidson’s opinion, which the Tribunal found reasonable, Dr. Kiss had administered a reasonable battery of tests, and there was sufficient testing for a psychological report.
19-009160 v MVACF: Considering the six factors outlined in the FSCO case of Al-Shimasawi v. Wawanesa, Vice Chair McGee found there was no new medical information to prompt the need for subsequent IEs. The prejudice the Respondent asserted it suffered as a result of the Applicant’s non-attendance was primarily a consequence of its own errors and missteps in adjusting the claim.

Tuesday Tips Archive
Challenging Opinions Where Records Not Reviewed
Q: The assessor did not review or reference the medical records that were provided to them in their opinion finding a treatment plan not reasonable and necessary. What search is optimal to find these cases?
Tip: Adding items from different filter categories functions as an “and” term and includes only hits containing all the items. However, adding multiple items within a category functions as an “or” term and includes each of those hits, even if not all together.
-
- Go to Keyword Search Enter – did not review
- Filter Results under Issues: Med
- Filter Results under Reason Code: Applicant’s Assessor Preferred
- Filter Results under Reason Code: Applicant’s Medical Records/CNRs
- Filter Results under Reason Code: Respondent’s Assessor Preferred
Results: 49 decisions on inHEALTH’s LAT Compendium
20-001512 v Unifund: In support of the physiotherapy Treatment Plan, the Applicant relied on the November 2019 report of Dr. Pathak, pain medicine specialist who recommended that the Applicant continue the various therapies. Adjudicator Kaur did not assign much weight to said report as he did not review any of the Applicant’s medical records. The Applicant reported that physical therapy alleviated his pain. However, this is different from what he had reported to Dr. Kopansky-Giles, chiropractor, a month prior at the IE. Moreover, the CNRs from Dr. Aziz months before the date of this Treatment Plan do not make any mention of pain-related complaints. The April 2019 report of Dr. WIlderman, chronic pain specialist, was also given little weight as Dr. Wilderman did not review the Applicant’s medical records. Accordingly, the Treatment Plan is not reasonable and necessary.
21-011242 v Aviva: Vice Chair Todd assigned Dr. Tu’s IE report little weight since she did not review any of the Applicant’s CNRs from treating physicians or the chronic pain assessment report, which was a significant omission. As such, the Applicant is entitled to the chronic pain assessment.
22-011557 v Security National: Adjudicator Mauro gave limited weight to Dr. Syed’s conclusion because, as argued by the Applicant, she did not review the progress report of social worker Ms. Mentz or previous OCF-18s. If she had reviewed them, Dr. Syed would have likely concluded that proceeding with social work treatment was necessary, as Ms. Mentz indicated that treatment enabled the Applicant’s ongoing progress and provided the required support to avoid client risk of re-injury, isolation, and deterioration of mental health and overall function. Moreover, the progress report of Ms. Mentz stated that the Applicant would learn strategies to manage stress, anxiety, and depressive symptomatology.

Credible Psych Reports
Q: Does not having psychological validity testing in an assessment affect the report’s credibility before the LAT when dealing with psychological impairments?
Tip: Find cases with issue-specific search filters to eliminate cumbersome keyword searches.
LAT Compendium Search
- Go to Issue/Benefit in Dispute
- Select Psych Validity Testing
Results: 124 decisions on inHEALTH’s LAT Compendium
16-000670 v Aviva: Adjudicator Truong preferred the medical evidence of the Respondent. Dr. Syed’s Psychological IE found no objective psychometric evidence of impairment and noted that the Applicant’s responses were “indicative of infrequent and atypical responding” as well as “feigning psychological impairment.” Little weight was given to the Applicant’s Psychological report by Dr. Pilowsky, as Dr. Pilowsky did not administer validity testing.
20-009840 v Travelers: Vice-Chair Brooks preferred the IE assessment by Psychologist Dr. A. Rubenstein, who concluded in December 2018 that the Applicant had no psychological impairments, and that the Applicant compromised the validity of psychological testing by amplifying her symptoms, because Dr. Rubenstein used clinical testing methods which enabled him to determine whether the Applicant was providing credible answers and Dr. Wagner did not administer validity testing.

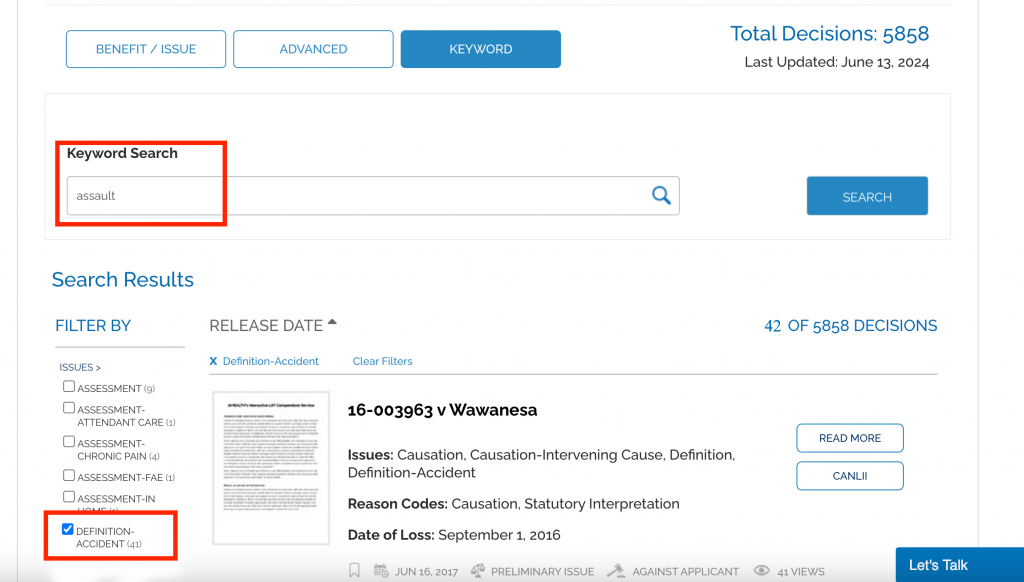
Definition Of Accident
Q: Can an assault involving a vehicle be considered an accident?
Tip: LAT Compendium Search
Keyword Search: Assault
Filter Results by ‘Issues’: Definition-Accident
Results: 41 decisions on inHEALTH’s LAT Compendium
Most Recent Decision: 23-013882 v Co-operators (July 18, 2024)
SABS Test: Facts must meet “Purpose” and “Causation” Tests
How to Demonstrate “Marked” Impairment
CAT Determination – Useful Factors for Marked Impairment
Q: What factors should be considered when assessing marked impairments that “significantly impede useful function” under Criterion 8?
Tip: Use keyword searches to isolate key strings in searches.
LAT Compendium Search:
1. Go to the Keyword Search
2. Search significantly impede useful function
Results: 8 decisions on inHEALTH’s LAT Compendium
SABS Test:
22-001654 v Wawanesa: Moderate impairments are compatible with “some” useful functioning. Marked impairments significantly impede “all” useful functioning.
20-001934 v Unica: It is important to accurately capture the applicant’s pre- and post-accident functions based on the totality of the medical and documentary evidence provided to determine the level of impairments for each of the four domains and whether these impairments, “significantly impede useful functioning.”
18-000605 v State Farm: The Tribunal prefers more thorough Occupational Therapy (OT) reports.
21-007794 v Co-operators: The Applicant must show that it is their psychological impairment which significantly impedes useful functioning, not their physical impairment.
18-000605 v State Farm: Credibility is important. It is necessary to look at the consistency in the information from the applicant’s testimony and that of their family members.
Looking for more decisions on CAT? Find all our CAT filters under issue in dispute.

IE’s: To Go or Not To Go?
Q: I need to find cases on the risk of not attending the Insurer’s Examination when I believe the Notice of Examination doesn’t provide sufficient reasons? If the Applicant attends the IE and it is determined the notice was insufficient, can the report be relied upon?
A: inHEALTH assists the researcher to narrow the search parameters based on the rationale/reasons they seek to have the report struck from the record. We can look at this question in a few different ways to help the researcher specify their searches.
- We can note that this question is related to cases dealing with whether Applicants have a right to dispute pursuant to s.55(1)2 when they do not attend IEs.
- We can look at cases where the Applicant attended the IE but sought to void the results based on the non-compliant notice.
- We narrowed the search to 21-004696 v Aviva where the Tribunal found that the Applicant’s right to challenge the insufficiency of an NOE was not waived by his attendance at the IEs, and the Tribunal did not consider the IE report based on the non-compliant notice.
Tip: Talk to your personal support team on Live Chat. We provide answers
-
- Go to Advanced Search
- Select Primary Criteria: “Referenced Cases/Legislation”
- Select: 21-004696 v. Aviva Insurance Company (Tribunal File Number 21-004696/AABS)
Results: 7 decisions on inHEALTH’s LAT Compendium
23-000568 v Allstate: Adjudicator Mohammed agreed with the Tribunal in 21-004696 that when a notice was deficient, the resulting IE was improper and that the results should not be considered. He further found the September 2022 IE was improper and the results would be given no weight.
22-000648 v Aviva: Adjudicator Jarda found that neither 21-004696 nor its reconsideration stood for the proposition that if an applicant attended an examination despite a non-compliant notice that any reports obtained from the examination would be void.
22-001864 v Aviva: Adjudicator Levitsky found that accepting the Applicant’s reasoning would lead to an absurd result where insureds could make a tactical decision to attend assessments, and if the assessment was not favourable, argue that the Treatment Plan was payable based on a technicality. She did not agree with the Tribunal’s statements in M.B. and 21-005696 that the Schedule makes no provision for an insured to be able to waive requirements under the Schedule, and only allows an insurer to do so. S. 44(6) allows the parties to mutually agree to waive a requirement for notice, and s. 46(2) allows an insured person to waive a conflict of interest with respect to a referral.

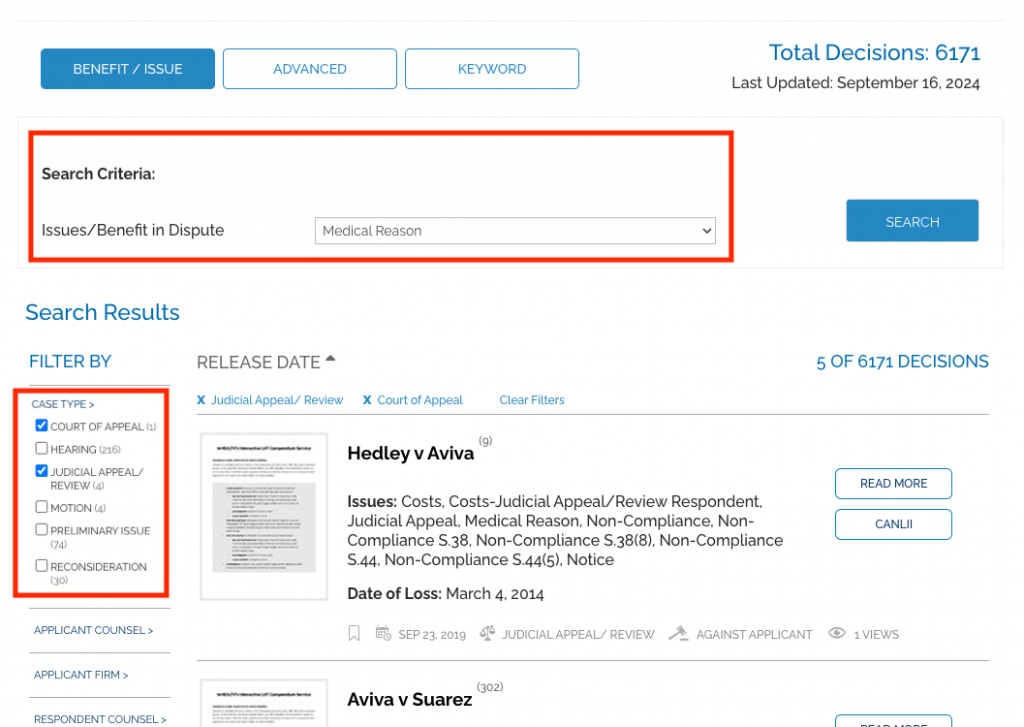
Medical Reasons
‘Mere Boilerplate’ Statements Are No Reasons At All
Sufficient “medical and any other reasons” have emerged as a significant part of handling accident benefit cases. The success rate when this issue is raised is 50/50, a key indicator of its importance to both parties.
An insurer is required to provide “medical and any other reasons” in 12 separate areas of the SABS.
The seminal LAT decision on the subject is M.B. v. Aviva (16-002325 v Aviva), but the Divisional Court and the Court of Appeal have also weighed in.
Tip: Filter by “Case Type” to find higher court decisions.
LAT Compendium Search:
1. Go to the Benefit/Issue Search
2. Set search criteria to Medical Reason
3. Filter Results by “Case Type”: Court of Appeal and Judicial Appeal/Review
Results: 5 decisions on inHEALTH’s LAT Compendium
SABS Test: Hedley v Aviva: Where reasons are required, they must be meaningful in order to permit the insured to decide whether or not to challenge the insurer’s determination. Mere “boilerplate” statements do not provide a principled rationale to which an insured can respond.
Post 104 IRB & Vocational Evaluations
Q: What factors does the Tribunal weigh when assessing vocational evaluations involving Post-104 IRB claims?
Section 6(2)(b) of the Schedule lays out the eligibility criteria for an IRB after the first 104 weeks of disability. Vocational evaluations are used to assist the parties and the Tribunal in determining if an Applicant has, as a result of the accident, a complete inability to engage in any employment or self-employment for which he is reasonably suited by education, training, or experience.
Tip: You don’t need to use quotation marks for the LAT Compendium Keyword search.
LAT Compendium Search
- Keyword Search: Go to Keyword Search
- Type vocational evaluation *(note: search vocational assessment for more results.)
- Filter Results by IRB-Post 104
Results: 14 decisions on inHEALTH’s LAT Compendium
16-000874 v Certas: The jobs identified by the Vocational Evaluation Report were entry-level minimum wage jobs which were not reasonably comparable to the Applicant’s previous employment in terms of wages, status or the work itself. Further, her Labour Market Analysis indicated relatively high unemployment rates for these jobs.
17-000889 v Travelers: The Adjudicator found Mr. Bachmann’s report to be “a thorough assessment of the applicant’s vocational history and functional limitations” and provided “an in-depth analysis supporting his conclusion that the applicant is unable to engage in any employment for which he is reasonably suited by education, training or experience”.
18-008937 v Certas: The Adjudicator found that the vocational evaluation report noted the Applicant’s lack of formal education, her lack of English skills and computer skills. It also included a transferable skills analysis and a comprehensive skills profile along with four suitable employment alternatives with compensation ranges for each, which were in line with her pre-accident income.
20-000143 v TD Insurance: The Vice-Chair did not find Ms. Billet’s IE vocational evaluation report or transferable skills analysis report appreciated how the Applicant’s psychological symptoms would affect her ability, mentally and physically, to engage in the types of occupations it proposed in light of her complaints about her inability to handle a rush and the anxiety that leads to her getting flustered and breaking down.
20-010511 v Wawanesa: The Panel placed less weight on the IE report of Vocational Evaluation Specialist Mr. Zervas because he was unable to identify any openings for the suggested roles in Northern Ontario, where the Applicant lived.
21-001592 v Intact: The Adjudicator accepted the findings of the Vocational Evaluation Report that the Applicant’s employability can only be accurately assessed when all factors (skill sets, chronic pain status, physical and cognitive limitations, emotionality, plus age) are considered.

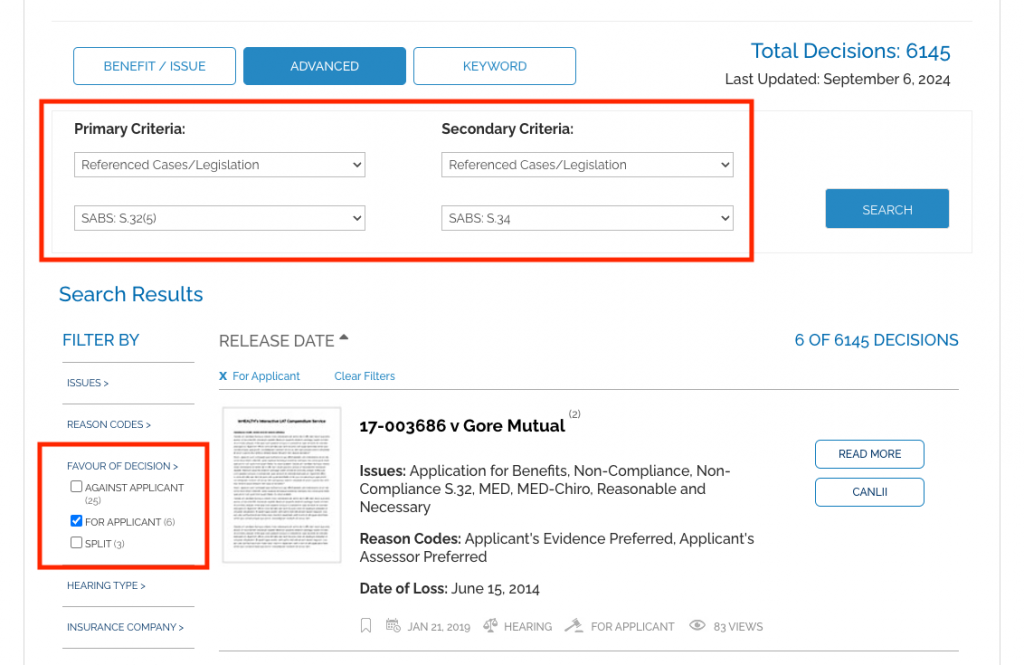
Reasonable Explanation
Q: When non-compliant with the 30 day time limit for submitting an OCF 1 Application for Accident Benefits as required under section 32(5) of the SABS, what constitutes a “reasonable explanation” under section 34?
Tip: Use Primary and Secondary searches to narrow your search results to find an answer.
LAT Compendium Search:
1. Go to Advanced Search
2. Set Primary Criteria to “Referenced Cases/Legislation”: SABS: S.32.5
3. Set Secondary Criteria to “Referenced Cases/Legislation”: SABS: S.34
4. Filter Results by “Favour of Decision”: For Applicant
Results: 6 decisions on inHEALTH’s LAT Compendium
Most Recent Decision: 23-014535 v Sonnet Insurance (August 7, 2024) The Tribunal found that, consistent with his examination under oath, the Applicant had limited familiarity with the accident benefits process, had limited English skills and was relying on his representative for his claim.
SABS Test: The guiding principles to what is a “reasonable explanation” are set out in Horvath v Allstate
Repaying ALL the IRBs Paid
Q: If an insured person being paid IRBs wilfully misrepresents his return to work, can he be compelled to repay all IRBs received or just those paid since his return to work?
Section 52(1)(a) of the Schedule provides for an insurer to be repaid benefits paid as a result of wilful misrepresentation or fraud. Our LAT Compendium search allowed us to quickly find that when an insured misrepresents their return to work, the insurer is entitled to repayment from the time they go back to work. However, if the insured does not demonstrate when they went back to work, the entire amount of IRBs paid may be ordered.
Tip: Use Primary and Secondary Criteria in our advanced search to find decisions containing both issues.
Talk to your personal support team on Live Chat. We provide answers
- Go to Advanced Search
- Select Primary Criteria “Issues”: Misrepresentation
- Select Secondary Criteria “Issues”: IRB-Repayment
- Filter results by “Favour of Decision”: For Applicant (in repayment cases, the insurer is often the Applicant.)
Results: 39 decisions on inHEALTH’s LAT Compendium
19-010729 v Unifund: The insurer was entitled to an IRB repayment of $4,431.14 due to the Respondent’s wilful misrepresentation of his return-to-work status for purposes of claiming IRB. He was ordered to refund IRBs starting from when he went back to work.
19-009392 v Aviva: The insurer was entitled to an IRB repayment of $5600. The Tribunal found that the insured failed to notify the insurer that he had returned to full-time duties as required by the Schedule and continued to collect payment of IRBs while no longer eligible, which amounts to a wilful misrepresentation. He was ordered to refund IRBs starting from when he went back to work.
20-000592 v Aviva: The insurer was entitled to IRB repayment of $36,456.00 for the period of May 12, 2017 to February 7, 2019 on the basis that the insured willfully misrepresented her return-to-work status. The Tribunal was unable to determine the applicable period of repayment as it did not accept the insured’s EUO evidence that she only returned to work in September 2018 given her inconsistent and perjurious testimony. Therefore, it found that the entire amount of IRBs paid was repayable.
19-008573 v Travelers: The Tribunal found that the insurer was entitled to a repayment of IRBs in the amount of $25,771.43 plus interest due to the Respondent’s wilful misrepresentation of her employment status. While there was a letter in evidence suggesting the insured went back to work in August 2016, the Tribunal ordered all IRBs paid going back to July 2016, In the absence of any submissions by the insured.
20-014898 v Certas: The insurer was entitled to repayment of $85,181.38, which was the full amount of IRBs paid, due to the insured’s willful misrepresentation and his failure to disclose records verifying his post-accident employment.

Rescheduling IE's
Q: What discretion does the Tribunal have to stay a proceeding and require insurers to allow an Applicant to attend a rescheduled IE?
S.55(2) of the Schedule permits the Tribunal to exercise its discretion to permit an Applicant to proceed with their claim before the Tribunal despite not complying with an IE pursuant to s.44. In these cases the Tribunal can stay the proceeding to allow the Applicant to attend, and may impose terms and conditions pursuant to s.55(3).
Tip: Filter search results on inHEALTH’s LAT Compendium by “Referenced Cases/Legislation” to zero-in on SABS section specific decisions.
LAT Compendium Search
- Go to Issue/Benefit in Dispute
- Select Non-Compliance S.44-Reschedule
- Filter Results by “Referenced Cases/Legislation”: SABS: S.55(2)
Results: 8 decisions on inHEALTH’s LAT Compendium
|
17-007683 v Aviva: Adjudicator Ferguson found that the Applicant’s explanations for failing to attend the IE were reasonable, and that the Respondent never disputed that such reasons were unreasonable or untruthful. The Respondent’s position “ignored the two cancellations for which written notice was provided. These events speak to the Applicant’s intention to comply with the Schedule and against any wilful non-compliance on her part. Pursuant to s.55(2) and (3) the Applicant must attend IEs required by the Respondent to assess IRBs and the Respondent must provide new IE dates within 35 days of the decision, and clearly set out the reasons for the rescheduled IEs. 19-001881 v Co-operators: The Tribunal found that the Applicant provided a reasonable explanation for her non-attendance at an IE as she did not receive notice of the IE from the Respondent or her counsel, and would have attended otherwise. Despite any prejudice to the Respondent the Tribunal found that barring the Applicant would be disproportionate, therefore she is allowed to proceed with her appeal once she attends the IE within 35 business days of the release of the decision. 18-011431 v Aviva: Given that the Applicant provided no reasonable explanation for her non-compliance with the Respondent’s IE request, Adjudicator Maleki-Yazdi declined to exercise the discretion afforded by s. 55(2). 20-013261 v Wawanesa: Adjudicator Watt found it would be unfair now under s.55(2) and (3) to grant permission for the Applicant to attend an examination, even with terms and conditions as The Respondent would be prejudiced now to have to try to assess any physical, psychological and vocational issues that might relate to IRB eligibility during the relevant time frame. 21-005342 v Intact: The Applicant’s entitlement to certain benefits hinges on a determination of whether he is catastrophically impaired, and fairness provides that, should he be, he has access to them as soon as possible. A dismissal at this stage would cause unnecessary delay by forcing him to reapply. It may be that after the completion of the IE a substantive hearing is not necessary. If it is necessary, a stay of proceedings allows the parties to contact the Tribunal to request a case conference to schedule a hearing, without unnecessary delay. |

What Cause is ‘Dominant’ in an Accident?
Q: There are many circumstances where the use or operation of an automobile can be considered an accident. What is the court’s interpretation of ‘intervening act’ when considering whether the facts meet the ‘definition of accident’?
As outlined in Economical v. Caughy, the causation test requires the adjudicator to determine if these “ordinary and well-known activities” were the direct cause of the Applicant’s impairments by focusing on the following considerations:
- The “but for” consideration;
- The intervening act consideration, which may serve to break the chain of causation where some other intervening events cannot be said to be part of the ordinary course of use or operation of the vehicle; and,
- When faced with a number of possible causes, the “dominant feature” consideration focuses on whether the ordinary and well-known activity is what most directly caused the injury.
Tip: Filter by “Judicial Appeal/Review” to find Divisional Court decisions.
LAT Compendium Search
- Go to Advanced Search
- Primary Search by “Issues/Benefit In Dispute”: Causation-Intervening Cause
- Secondary Search by “Issues/Benefit In Dispute”: Definition-Accident
- Filter Results under Case Type: Judicial Appeal/Review
Results: 7 decisions on inHEALTH’s LAT Compendium
Porter v Aviva: “Legal entitlement to accident benefits requires not just that the use or operation of a car be a cause of the injuries, but that it be a direct cause.” In this case, the dominant factor that caused Ms. Porter’s injuries was the icy, snow-covered driveway, and the use or operation of the Lyft car was “at best ancillary”, but not a direct cause of the injuries.
Sajid v Certas: The Court of Appeal noted in Greenhalgh v. ING Halifax, the “but for” test can act as a useful screen,” but in some cases, “the presence of intervening causes may serve to break the link of causation where the intervening events cannot be said to be part of the ordinary course of use or operation of the automobile.”
Jiang v Co-operators: In applying the “intervening cause” test, Adjudicator Kaur erred by ignoring there were two phases to the incident: injuries allegedly caused by an assault and injuries allegedly arising from the subsequent loss of control of the vehicle. Adjudicator Kaur failed to give reasons for why the road accident was also not a direct cause of the injuries.
Davis v Aviva: The black ice the Applicant slipped on was fortuitous, but not an intervening cause or event. The Applicant had the electronic key fob in her hand to open and enter her car, which was a part of the use of a motor vehicle. She was so close to completing that entry that her leg came to rest under the front wheel on the driver’s side. “Referring to the reasoning in Seung, the presence of the key fob was a fact that supported the finding that the use of the car was the direct cause of her fall, not the ice beneath her feet”.

Let inHEALTH’s Experience Work for You
With 6,000+ LAT decisions reviewed, indexed, summarized – We know stuff.
Our Team Is Here To Help!
1
Select your
service
2
Ask your question
3
Our Team provides answers
Get Started here